Overview
The article highlights the emotional challenges faced by nurse practitioners in their daily roles, particularly the administrative burdens that can detract from patient care. It emphasizes the importance of structured documentation, specifically SOAP notes, as a means to alleviate these pressures. By providing comprehensive examples, it showcases how well-organized SOAP notes can enhance communication among healthcare providers.
Imagine the relief of knowing that all relevant information is accurately captured and easily accessible. This not only improves patient outcomes but also fosters a collaborative environment where everyone is on the same page. When healthcare professionals feel confident in their documentation, they can focus more on what truly matters—their patients.
As you reflect on your own experiences, consider how implementing structured SOAP notes could transform your practice. The benefits are clear:
- Improved communication
- Enhanced patient care
- A more efficient workflow
We encourage you to embrace this approach and explore the resources available to support you in this journey.
Introduction
In the fast-paced world of healthcare, the ability to document patient interactions efficiently is more crucial than ever. Nurse practitioners often grapple with the dual pressures of providing quality care while managing extensive administrative tasks, which can lead to feelings of overwhelm and potential burnout. This article delves into ten comprehensive SOAP note examples tailored for nurse practitioners, showcasing how structured documentation can enhance patient care and streamline workflows.
As the demands of clinical practice evolve, how can practitioners ensure their note-taking remains both effective and efficient amidst these challenges? By reflecting on these questions, we can explore solutions that not only alleviate stress but also improve the quality of care provided to patients.
CosmaNeura: AI-Driven SOAP Note Automation for Nurse Practitioners
In today’s healthcare landscape, many practitioners face overwhelming emotional challenges. The burden of administrative tasks can lead to burnout, detracting from the quality of patient care. CosmaNeura understands these struggles and offers a compassionate solution.
By harnessing cutting-edge AI technology, CosmaNeura streamlines the generation of clinical records. This innovation significantly reduces the time nurse practitioners spend on paperwork, allowing them to focus more on meaningful interactions with their patients. Imagine being able to dedicate more time to those who matter most, rather than getting lost in administrative duties.
The platform integrates client data and clinical insights to generate a comprehensive soap note example nurse practitioner that is both precise and thorough. This not only enhances efficiency but also ensures adherence to best practices in documentation, aligning with the ethical standards of Catholic teachings. By alleviating the administrative burden, CosmaNeura empowers healthcare providers to deliver quality care without compromising their values.
In addressing these critical healthcare challenges, CosmaNeura promotes a faith-focused approach to care for individuals. Are you ready to embrace a solution that nurtures both your professional and personal well-being? Join us in transforming the way you deliver care.
Heidi Health: Comprehensive SOAP Note Template with Examples
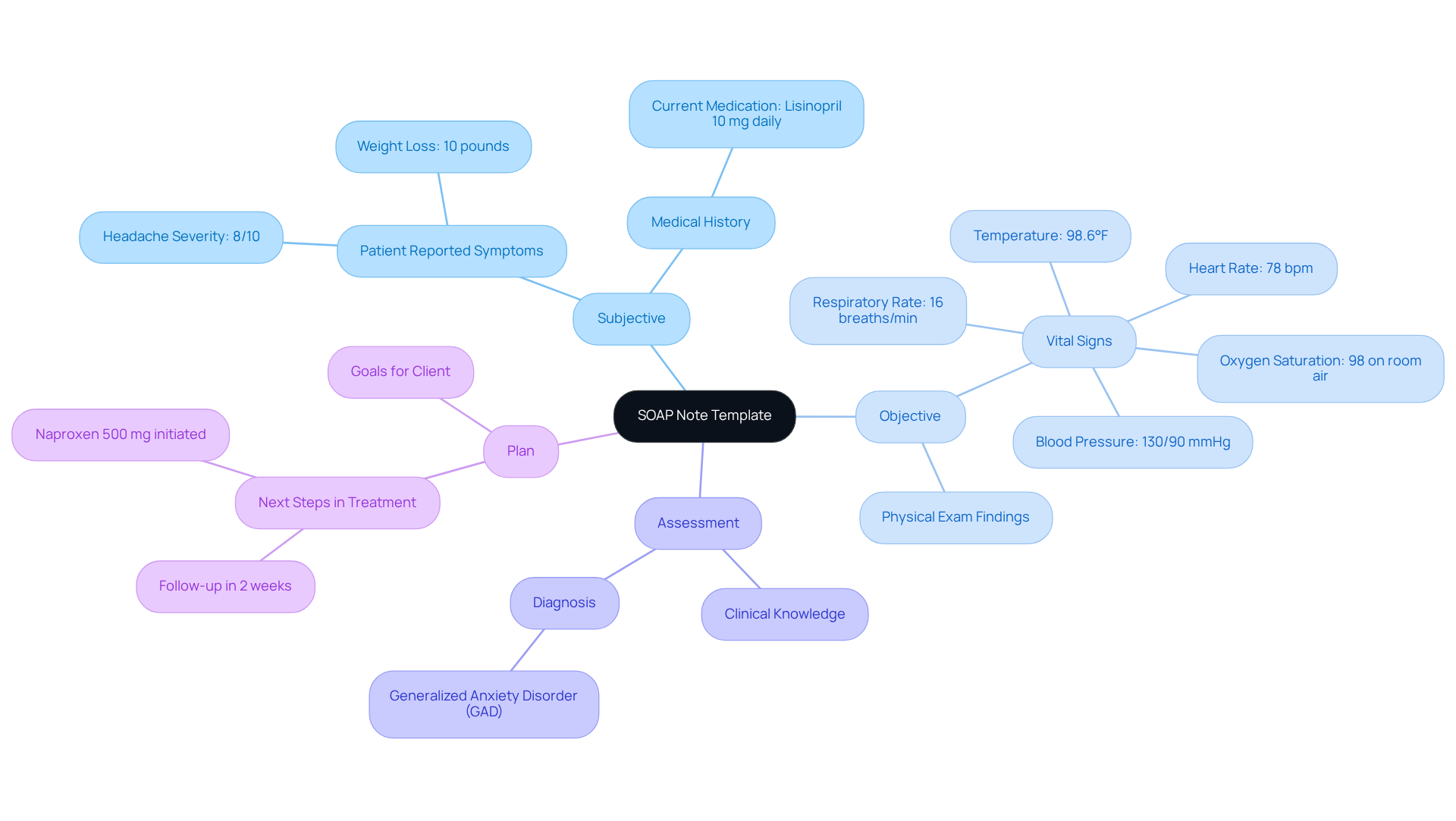
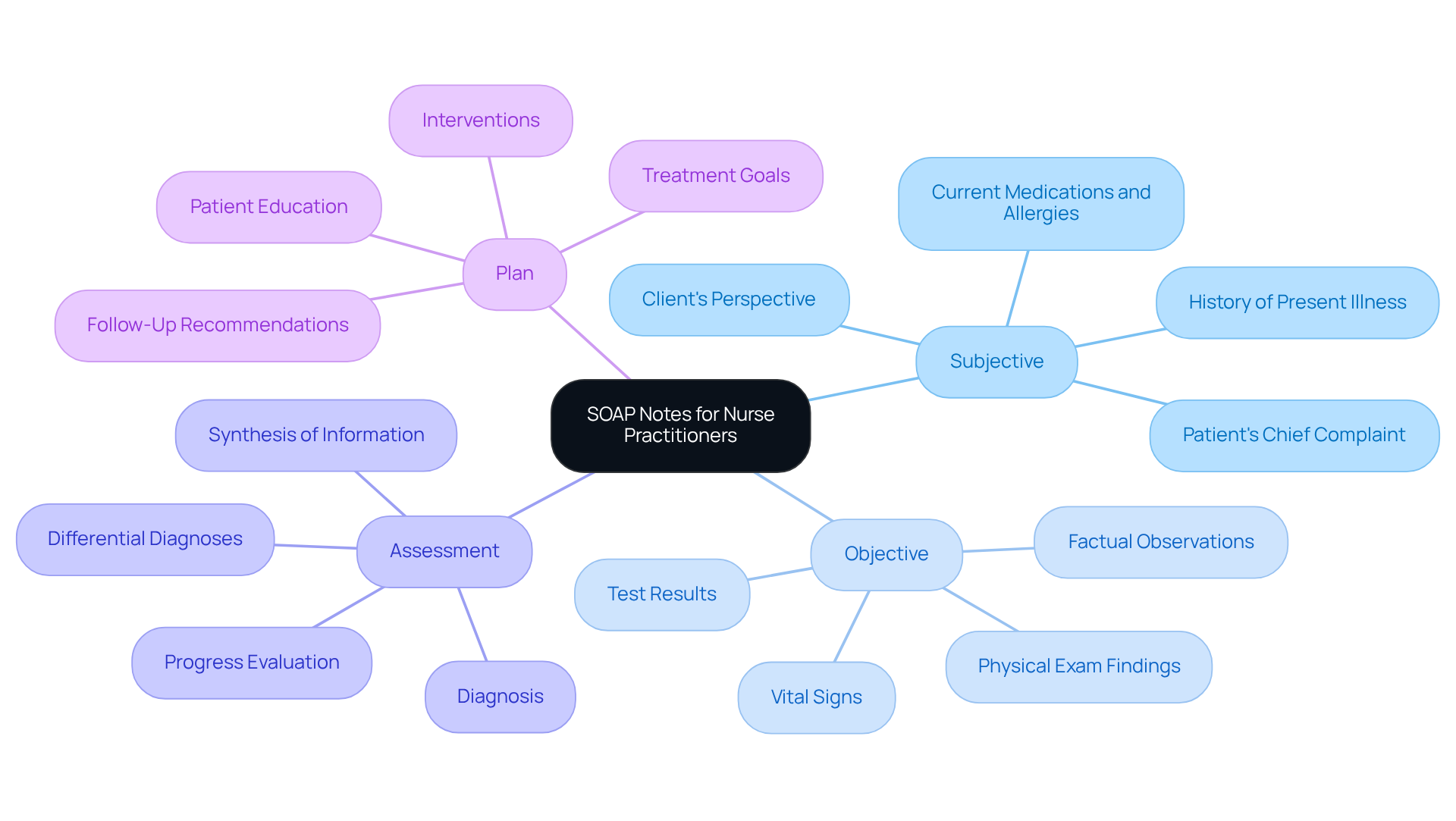
Heidi Health understands the emotional challenges healthcare providers face with documentation. The administrative burdens can feel overwhelming, impacting the quality of patient care. That’s why we offer a comprehensive soap note example nurse practitioner that efficiently organizes interactions into four main sections: Subjective, Objective, Assessment, and Plan. Each section is crafted to capture essential information, ultimately enhancing the quality of documentation and care for individuals.
Consider the Subjective section, where a nurse practitioner might document an individual’s reported symptoms, such as a headache rated 8 out of 10 over the past three days. The Objective section complements this by including measurable data, like vital signs—a blood pressure reading of 130/90 mmHg and a heart rate of 78 bpm—along with physical exam findings. This structured format ensures that all relevant information is meticulously recorded, facilitating better communication among healthcare providers and leading to improved patient outcomes.
By following current best practices in the comprehensive soap note example nurse practitioner, practitioners can streamline their processes, reduce errors, and enhance the overall quality of care. Notably, Priority Physicians reported a 70% reduction in charting time within just 14 weeks of utilizing AI software such as Heidi, highlighting the efficiency achieved through organized record-keeping.
Furthermore, integrating generative AI into the documentation process allows healthcare providers to automate repetitive tasks. This shift enables them to focus more on patient interactions and engagement. Effective documentation can significantly improve the quality of care offered to clients, making training in this writing technique essential for new practitioners.
How can you enhance your documentation practices today? Reflect on the benefits of structured note-taking and consider how it can transform your patient care experience.
Nursing Process: Step-by-Step Guide to Writing Effective SOAP Notes
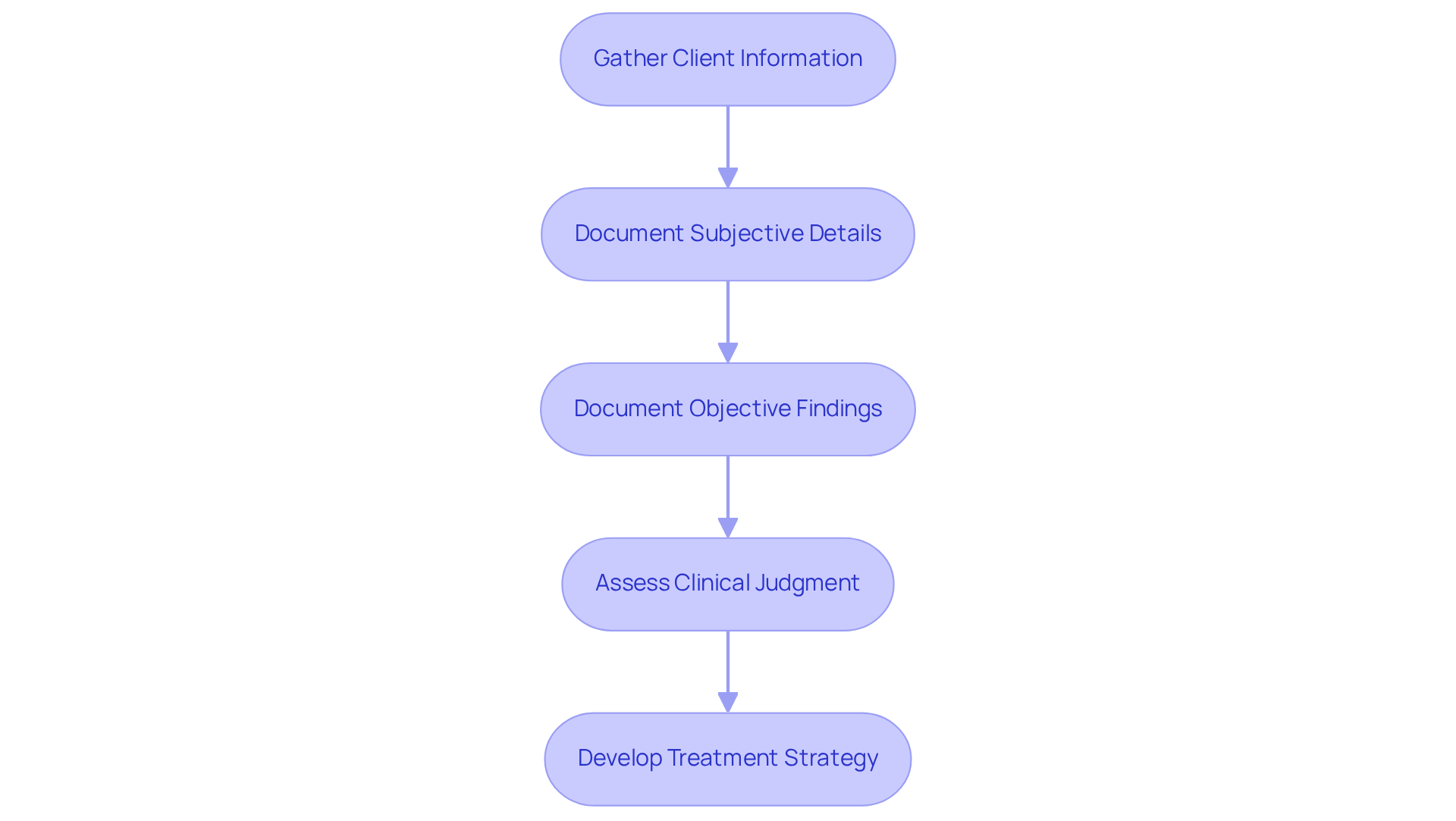
The nursing process is essential for creating effective documentation, and it involves several key steps that can significantly impact patient care. Have you ever felt overwhelmed by the amount of information you need to gather? Start by collecting thorough client information through detailed interviews and evaluations. Once you have this information, arrange it into a structured format: document subjective details reported by the individual, objective findings from physical examinations, assessments derived from clinical judgment, and a clear treatment strategy.
This systematic approach not only enhances the quality of records but also improves patient outcomes by ensuring that all relevant information is meticulously considered in care planning. For instance, utilizing tools such as the OLDCARTS acronym can assist in structuring the History of Present Illness (HPI). Remember, keeping brevity in documentation is essential for clarity and focus.
Additionally, it's crucial to be aware of the challenges posed by electronic documentation, such as data overload. How can we ensure effective note-taking amidst these challenges? By following these best practices, nurse practitioners can create a comprehensive soap note example nurse practitioner that ensures detailed and efficient documentation, fostering communication and continuity of care. Your dedication to this process makes a significant difference in the lives of your patients.
Studying Nurse: Diverse SOAP Note Examples for Various Clinical Situations
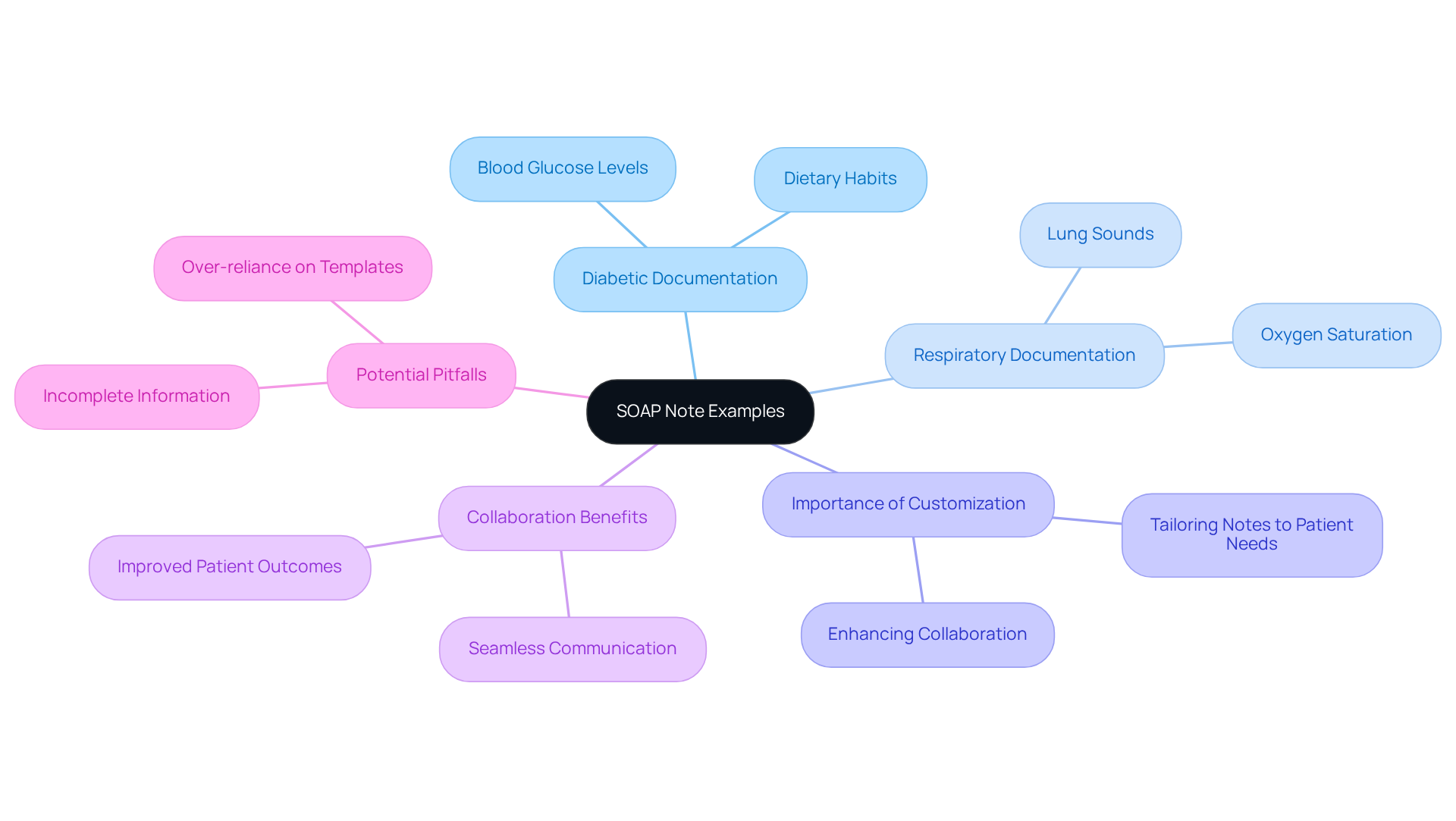
Studying Nurse offers a comprehensive soap note example nurse practitioner that serves as a thoughtful compilation of documentation examples addressing various clinical scenarios, from routine check-ups to complex cases. Have you ever felt overwhelmed by the details? For instance, documenting for a diabetic individual may include specific details about blood glucose levels and dietary habits, while a record for someone with respiratory issues would focus on lung sounds and oxygen saturation, like a blood pressure reading of 152/90. These examples illustrate the flexibility of the format and encourage nurse practitioners to adapt their records to meet unique client situations.
As Courtney Gardner wisely notes, a comprehensive soap note example nurse practitioner offers a swift and organized method to document your client’s treatment, refresh your memory regarding previous sessions, and enable smooth cooperation with colleagues. This customization not only enhances the significance of their annotations but also fosters collaboration among healthcare teams, ultimately leading to better outcomes for patients. Moreover, timely records are crucial; they minimize errors and ensure that all relevant patient information is accurately captured.
However, it’s important for practitioners to be mindful of potential pitfalls in their records. Incomplete information or an over-reliance on templates can compromise the quality and effectiveness of their entries. By recognizing these challenges and taking proactive steps, healthcare providers can enhance their documentation practices and, in turn, improve patient care.
Clincepts: Common Mistakes in SOAP Note Documentation and How to Avoid Them
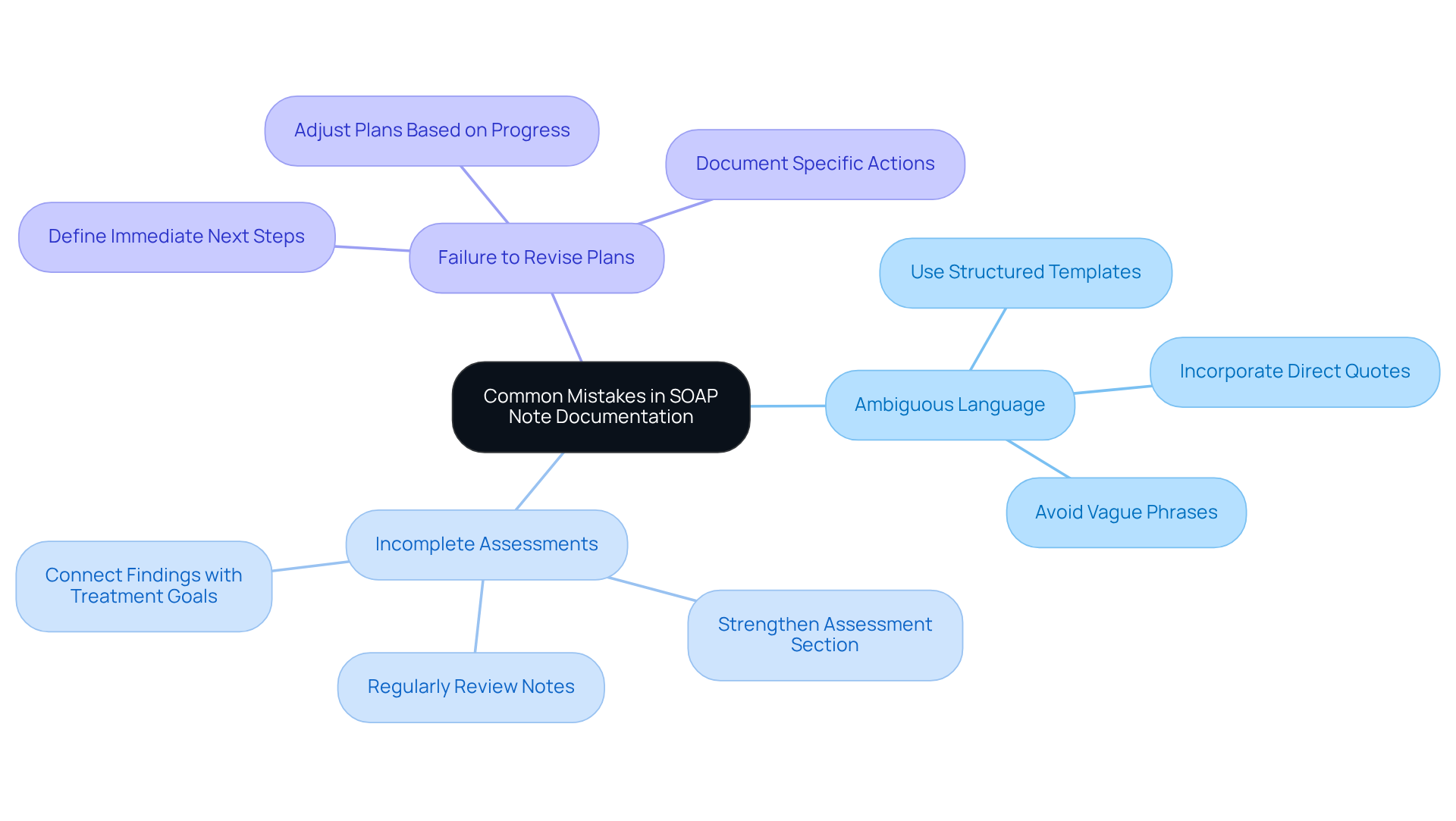
Clincepts identifies several common errors in SOAP documentation, such as ambiguous language, incomplete assessments, and the failure to revise plans based on client progress. These challenges can be emotionally taxing for healthcare providers, who strive to deliver the best care possible. To address these concerns, nurse practitioners should prioritize precision in their records by creating a comprehensive soap note example nurse practitioner that accurately reflects the individual's current condition.
For example, incorporating direct quotes from individuals in the Subjective section can enhance authenticity and clarity. Have you considered how this simple practice could transform your documentation? Consistently examining and updating notes is essential for maintaining precision and relevance. Research shows that record mistakes can significantly affect care outcomes for individuals. A decade-long retrospective study revealed that 20% of medical malpractice cases included at least one record-keeping error, underscoring the critical need for accurate records.
By adopting structured templates and focusing on quantifiable data, practitioners can elevate the quality of their records, as demonstrated in a comprehensive soap note example nurse practitioner. This approach not only improves patient care but also fosters better communication among healthcare teams. As highlighted by HealthOrbit AI, one of the most frequent errors is overgeneralizing in the Subjective section, which can weaken the impact of the records.
Consider these key solutions to enhance your documentation:
- Use structured templates to guide your entries.
- Incorporate direct quotes to add authenticity.
- Regularly review and update your notes.
By taking these steps, you can ensure that your records are not only accurate but also a true reflection of the care you provide.
NP Charting School: Practical SOAP Note Examples for Nurse Practitioners
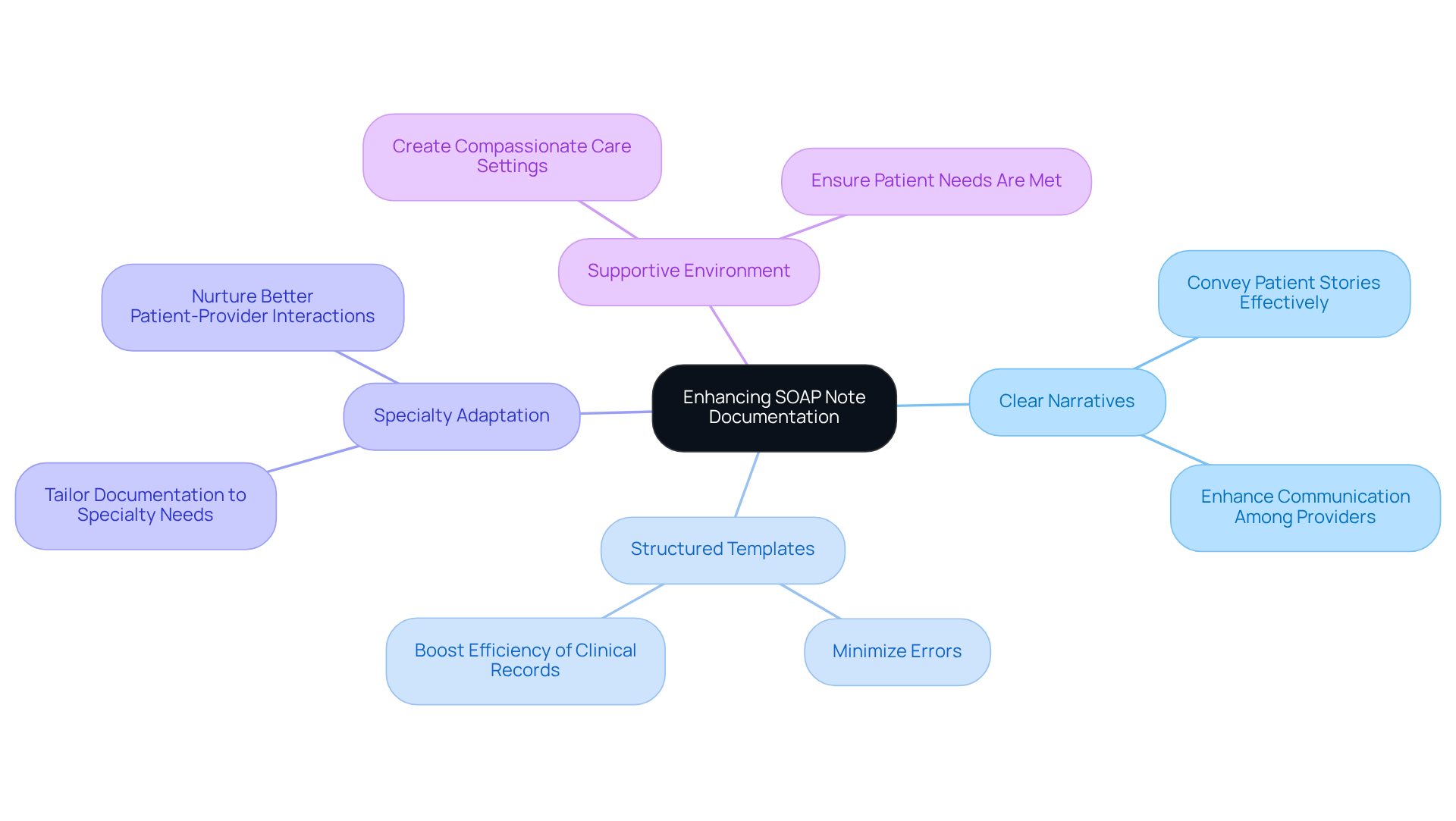
The NP Charting School recognizes the emotional challenges faced by nurse practitioners in their daily routines. We provide a comprehensive soap note example nurse practitioner, along with practical documentation examples tailored for various specialties, including pediatrics, geriatrics, and mental health, to alleviate some of the burdens that can impact patient care. Each comprehensive soap note example nurse practitioner is thoughtfully designed to highlight essential components of effective record-keeping, such as clear individual narratives and well-defined care plans.
By exploring these instances, nurse practitioners can enhance their record-keeping skills, ensuring their structured summaries serve as a comprehensive soap note example nurse practitioner that is not only informative but also actionable. Present trends in record-keeping practices underscore the importance of clarity and accuracy, which are vital for fostering better communication among healthcare providers and improving patient care outcomes.
Moreover, research indicates that utilizing organized templates significantly reduces errors and boosts the overall efficiency of clinical records. Specialty-specific guidance included in these examples helps practitioners tailor their documentation to meet the unique demands of their fields, ultimately nurturing better patient-provider interactions and care continuity.
Consider these key solutions to enhance your record-keeping:
- Utilize clear narratives to convey patient stories effectively.
- Implement structured templates to minimize errors.
- Adapt documentation practices to fit your specialty's needs.
By embracing these strategies, you can create a more supportive environment for your patients, ensuring their needs are met with compassion and professionalism.
Berxi: The Importance of SOAP Notes in Nursing Documentation
Berxi emphasizes the vital role of clinical records in nursing reports, serving not only as a legal account of care provided but also as a means for effective communication among healthcare professionals. Have you ever felt the weight of ensuring continuity of care? A comprehensive soap note example nurse practitioner serves as documentation that provides a clear and concise overview of patient interactions, evaluations, and treatment strategies, helping to alleviate some of that burden.
This written material is crucial for clinical decision-making and ensuring compliance with regulatory standards, protecting practitioners in case of disputes. Larry Weed proposed a structured documentation format nearly 50 years ago, underscoring its lasting significance in clinical practice. Efficient record-keeping through structured summaries, such as a comprehensive soap note example nurse practitioner, can significantly reduce legal risks, as comprehensive accounts are essential for justifying clinical choices in malpractice cases.
As Kunal Sindhu, MD, notes, ineffective communication is among 'the most frequent identifiable reasons for sentinel events.' This highlights the importance of clear records in preventing legal issues. By maintaining a comprehensive soap note example nurse practitioner, healthcare professionals can demonstrate adherence to documentation standards, ultimately fostering a safer and more responsible healthcare environment.
Furthermore, the APSO order has been shown to enhance speed and usability during chronic disease visits, improving care efficiency. Let’s embrace the power of meticulous documentation—it not only protects us but also enriches the care we provide to our patients.
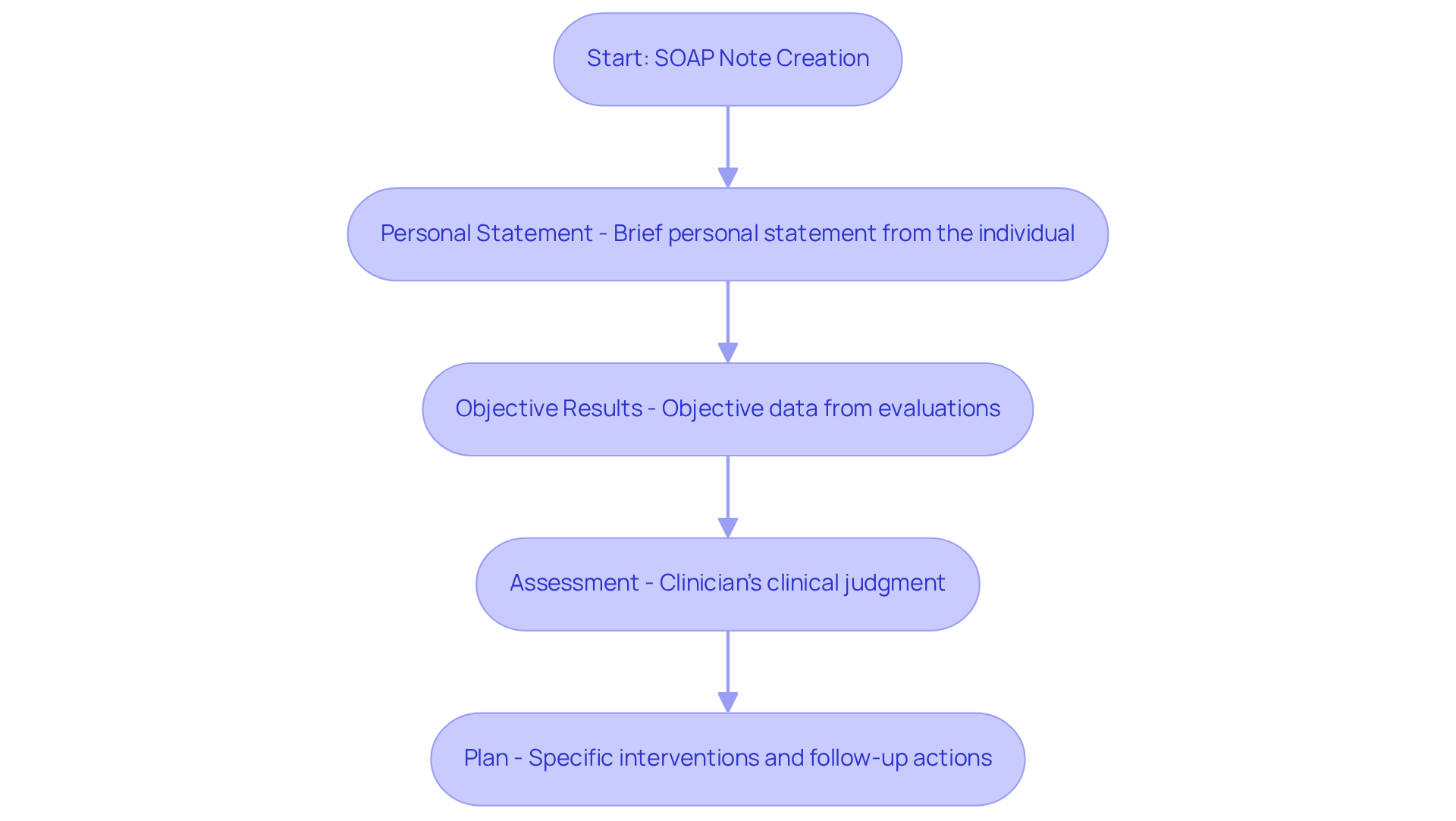
AskJAN: Key Components of Effective SOAP Notes for Healthcare Providers
In the demanding world of healthcare, efficient documentation can often feel overwhelming. Have you ever felt the weight of administrative tasks overshadowing the time you wish to spend with your patients? AskJAN highlights essential elements that can ease this burden, focusing on a clear format, pertinent client information, and actionable strategies.
Every clinical document should begin with a brief personal statement from the individual, followed by objective results from evaluations. This structure not only streamlines the process but also ensures that the patient’s voice is heard. The assessment section should reflect the clinician's clinical judgment, while the plan outlines specific interventions and follow-up actions. By adhering to these elements, nurse practitioners can develop a comprehensive soap note example nurse practitioner that is not only informative but also supportive of continuous care.
Imagine the impact of well-organized documentation on your workflow and patient relationships. By following these guidelines, you can enhance the quality of care you provide, making your interactions more meaningful. Let’s work together to transform the documentation process into a tool that fosters better patient outcomes and lessens your administrative burden.
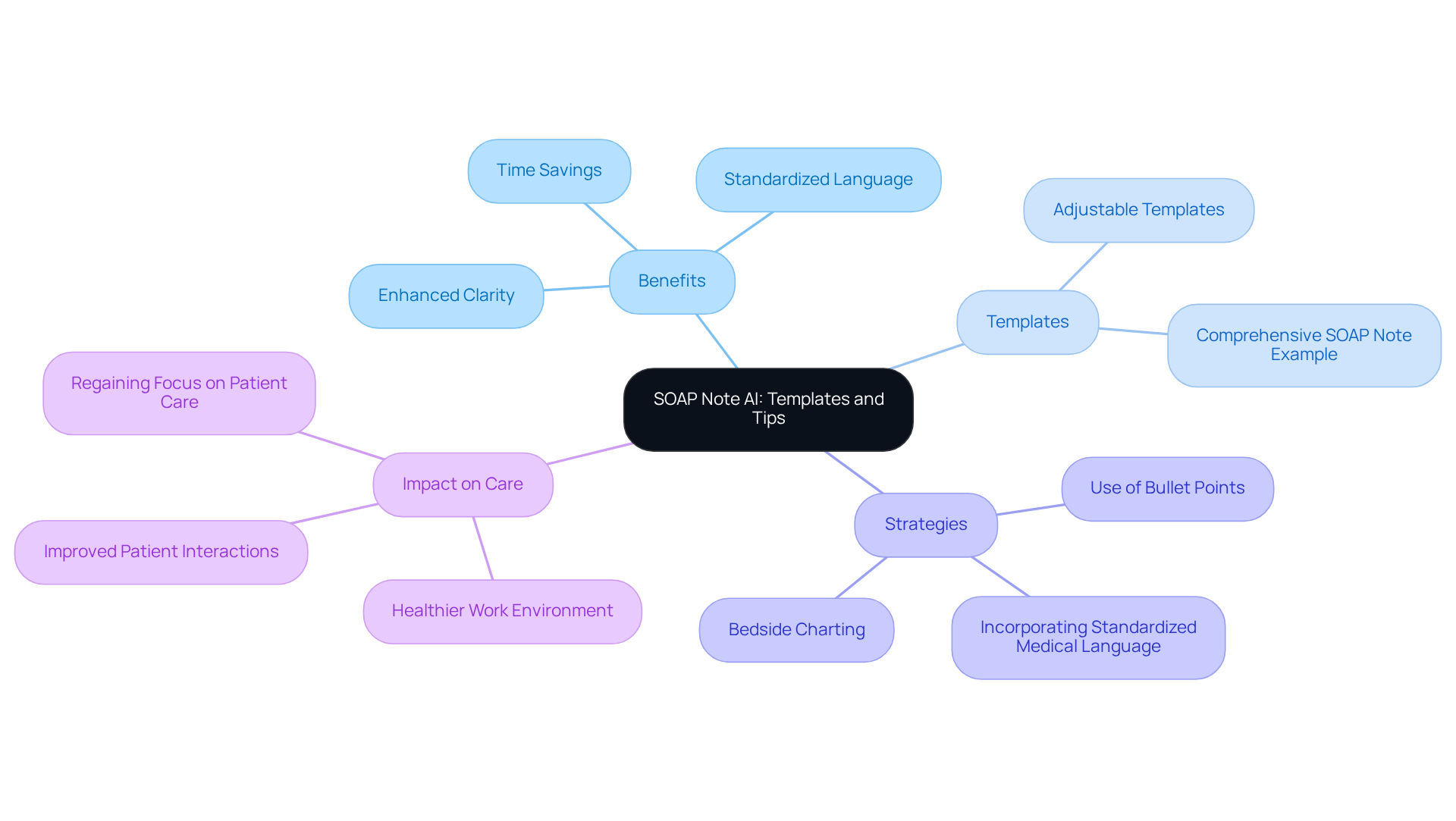
SOAP Note AI: Templates and Tips for Efficient SOAP Note Writing
Healthcare providers often face overwhelming emotional challenges due to administrative burdens, which can detract from their ability to provide quality patient care. SOAP Note AI understands these struggles and offers a range of adjustable templates and effective strategies, including a comprehensive soap note example nurse practitioner, designed to enhance the SOAP writing process. By addressing various clinical situations, these templates serve as a comprehensive soap note example nurse practitioner, empowering them to efficiently record interactions while maintaining high standards of quality.
Imagine being able to use bullet points for enhanced clarity and incorporating standardized medical language that promotes consistency across notes. This not only simplifies documentation efforts but also significantly decreases the time needed for record-keeping. As a result, healthcare providers can regain precious hours to focus on what truly matters—the direct care of individuals.
By using a comprehensive soap note example nurse practitioner, practitioners can enhance their focus on delivering outstanding experiences for those receiving care. This shift not only enhances patient interactions but ultimately contributes to a healthier work environment in the healthcare sector. Are you ready to take a step towards reducing administrative burdens and enhancing your practice? Embrace the support that SOAP Note AI offers and transform your documentation process today.
Amazon: Essential Guide to Understanding SOAP Notes for Nurse Practitioners
Amazon provides a crucial manual that explains the basics of clinical documentation, including its purpose, structure, and best practices. This guide serves as a comprehensive soap note example for nurse practitioners, offering insights into how to effectively document care for individuals. Have you ever felt overwhelmed by the demands of documentation? By grasping the importance of every element of the Subjective, Objective, Assessment, and Plan structure, practitioners can enhance their record-keeping abilities and ensure that their observations positively impact patient outcomes.
Documentation is vital for continuity of care, billing/coding, and legal protection. As noted by Team Simply.Coach, "Effective documentation through structured records ensures that you remain organized and consistent in monitoring progress, interventions, and treatment modifications." This guide emphasizes clarity, conciseness, and relevance in each section, aiding practitioners in creating a comprehensive soap note example nurse practitioner that is effective.
Imagine the peace of mind that comes with knowing your documentation is thorough and impactful. By embracing these best practices, you can not only alleviate some of the administrative burdens but also improve the quality of care you provide. Let this guide empower you to navigate the complexities of clinical documentation with confidence and compassion.
Conclusion
Efficient documentation is not just a task; it’s a lifeline in the nursing profession, especially when it comes to SOAP notes. These structured records are essential for fostering communication among healthcare providers and enhancing the quality of patient care. By utilizing comprehensive SOAP note examples tailored to various clinical situations, nurse practitioners can ease the administrative burdens that often overshadow their primary focus—patient interaction.
Throughout this article, we’ve explored vital insights about the significance of organized and precise documentation. The advantages of AI-driven solutions like CosmaNeura and Heidi Health, along with practical examples from Studying Nurse and NP Charting School, underscore the necessity of effective SOAP note writing for improving patient outcomes. Moreover, recognizing common pitfalls and adopting best practices can lead to more accurate and meaningful records, ultimately nurturing better communication within healthcare teams.
As the demand for quality patient care continues to rise, embracing efficient documentation practices is more important than ever. Nurse practitioners are encouraged to delve into the tools and strategies discussed—ranging from structured templates to AI automation—to refine their documentation processes. By prioritizing effective SOAP note writing, healthcare providers can not only enhance their workflow but also contribute to a more compassionate and efficient healthcare environment.




